Innovative T Cell Therapy: A New Hope for Type 1 Diabetes
Written on
Chapter 1: The Promise of Engineered T Cells
For those diagnosed with type 1 diabetes, a transformative therapy is on the horizon, leveraging genetically altered immune cells. Researchers at the Seattle Children’s Research Institute’s Center for Immunity and Immunotherapies have secured a substantial research grant aimed at expediting the clinical application of this innovative treatment.
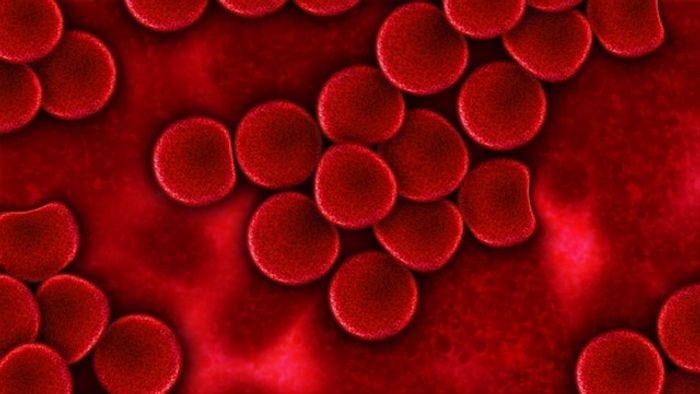
In cases of type 1 diabetes, the pancreas fails to produce adequate insulin, which is critical for regulating blood sugar levels. This deficiency arises from a specific type of white blood cell, known as effector T cells, which invade the pancreas and destroy the insulin-producing islet cells.
Regulatory T cells play a crucial role in managing the activity of effector T cells, signaling them to moderate their response and minimize damage to pancreatic tissues.
Patients lacking sufficient insulin frequently experience fatigue, extreme thirst, excessive hunger, and unintended weight loss, even when their eating habits remain unchanged. By the time type 1 diabetes is identified, approximately 80 to 90 percent of the islet cells may have sustained irreversible damage.
In healthy individuals, regulatory T cells, or Tregs, effectively suppress the activity of effector T cells. According to David Rawlings, the lead investigator on this research, these Tregs are essential for preventing excessive tissue damage.
In a study published in Science Translational Medicine, Rawlings and his team devised a groundbreaking method to restore the balance between effector and regulatory T cells. This process involves isolating a patient’s own T cells from a blood sample, genetically modifying them to imbue Treg-like properties, and then reinfusing them into the patient. This allows the modified T cells to inhibit the overactive effector cells in the pancreas and protect the organ from further harm.
The research revealed the first evidence that activating the FOXP3 gene can yield T cells that function similarly to regulatory T cells. The team discovered that by switching on this specific gene, the modified T cells exhibited characteristics akin to Tregs in both animal studies and tissue cultures.
“This data provides the first evidence that engineering T cells by activating FOXP3 can produce a functional Treg-like cell,” stated Rawlings, emphasizing the clinical relevance of this important discovery.
Rawlings and his colleagues are optimistic that this pioneering technology presents considerable benefits over existing treatments for type 1 diabetes, as well as other therapies aimed at enhancing Treg function. Their immediate focus is on further validating this therapy and establishing clinical protocols for its application.
“I believe there were doubts within the field regarding the efficacy of our approach, so it is rewarding not only to confirm that it works but also to continue accumulating data demonstrating its remarkable effectiveness,” Rawlings expressed.
Chapter 2: Video Insights into Diabetes Cell Therapy
This video, titled "Easing Pain, Restoring Lives: Preventing Diabetes with Islet Cell Transplantation," offers an in-depth look at the advancements in diabetes treatment through innovative therapies. It explores how islet cell transplantation can significantly improve the quality of life for individuals living with diabetes.